
All you wanted to know about craniofacial surgery and didn’t know who to ask
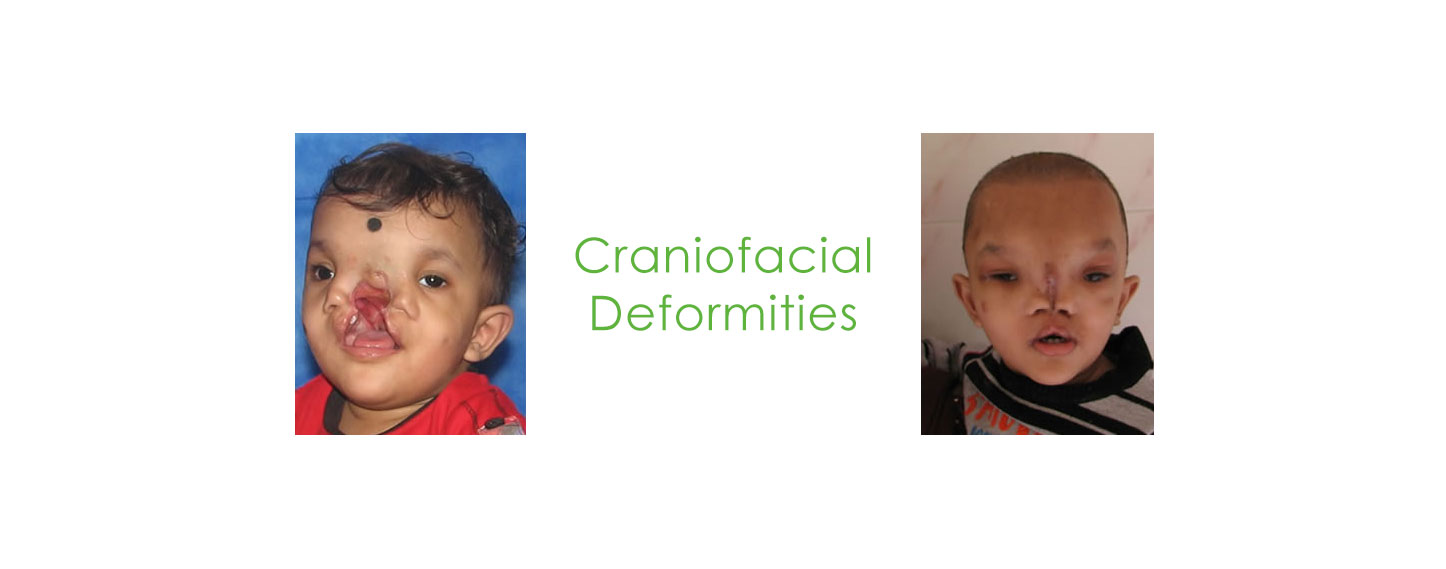
Craniofacial surgery is a surgical subspecialty of plastic surgery and oral and maxillofacial surgery that deals with congenital and acquired deformities of the head, skull, face, neck, jaws and associated structures. Although craniofacial treatment often
involves the manipulation of bone, craniofacial surgery is not tissuespecific, i.e., craniofacial surgeons deal with bone, skin, nerve, muscle, teeth, among others. Defects typically treated by craniofacial surgeons include craniosynostosis, rare
craniofacial clefts, acute and chronic sequellae of facial fractures, cleft lip and palate, micrognathia, Treacher Collins Syndrome, Apert’s Syndrome, Crouzon’s Syndrome, hemifacial microsomia and many others.

Almost 15,000 children are born with such deformities (congenital craniofacial anomalies) each year in India.

Training in craniofacial surgery usually consists of a surgical fellowship completed after a residency in either
plastic surgery, oral and maxillofacial surgery, or otolaryngology. There are less than 10 active craniofacia
surgeons in India and less than 100 across the world.

Pioneered in 1968, surgery has become easier in planning and execution due to advances in imaging technologies and making external models of the skull and the face down to the exact detail to simulate the surgery prior to the actual procedure.
The use of endoscopes, resorbable plating systems, 3D planning software and of course high-end operation theatres and ICUs have made the surgery safe. This has made it possible for most patients to be operated at the age of less than a year. In case
of some deformities where one needs to lengthen the bone using specialised devices, the surgery can be performed the day the baby is born. The result is that the child can be returned to a normal life with no evident (or marginal) facial deformity.

In cases where the forehead is involved (trigonocephaly and plagiocephaly), a technique called fronto-supraorbital advancement is used to correct the shape of the head. The procedure is performed at a young age in order to provide the brain with enough space to grow and prevent abnormal skull growth. Fronto-orbital advancement literally means moving the front of the skull, including the eye sockets, forward. A section of the skull, ranging from the coronal sutures to the eye sockets is cut loose in order to correct the shape of the skull. The incision is cut in a zigzag shape from ear to ear so that the hair will cover the scar and make it less visible. The incision is
made to the bone only, leaving the underlying meninges intact. The top half of the eye sockets is cut loose. Once the eye socket section has been cut loose, a vertical incision is made in the midline, and the whole section of the eye socket is bent outwards in order to correct the pointed shape of the forehead. Because the section is now too wide, a wedge needs to be cut on either side to allow the section to fit into the skull.
In scaphocephaly the sagittal suture is prematurely fused, preventing the skull from growing perpendicular to the suture. Thus the head becomes narrow and long. If a scaphocephaly is diagnosed within 4 to 5 months
after birth, it can be corrected with a relatively simple procedure, whereby the saggital suture is surgically reopened. Once the suture has been opened, the bone segments can grow again and the head can regain its normal shape. This operation is only performed on patients younger than five months old with a scaphocephaly. This is due to the fact that the bone segments only have the ability to adapt so severely when the operation is performed at this young age. A scaphocephaly that is diagnosed and treated later in life requires a more extensive secondary operation than one which is treated before eight months.

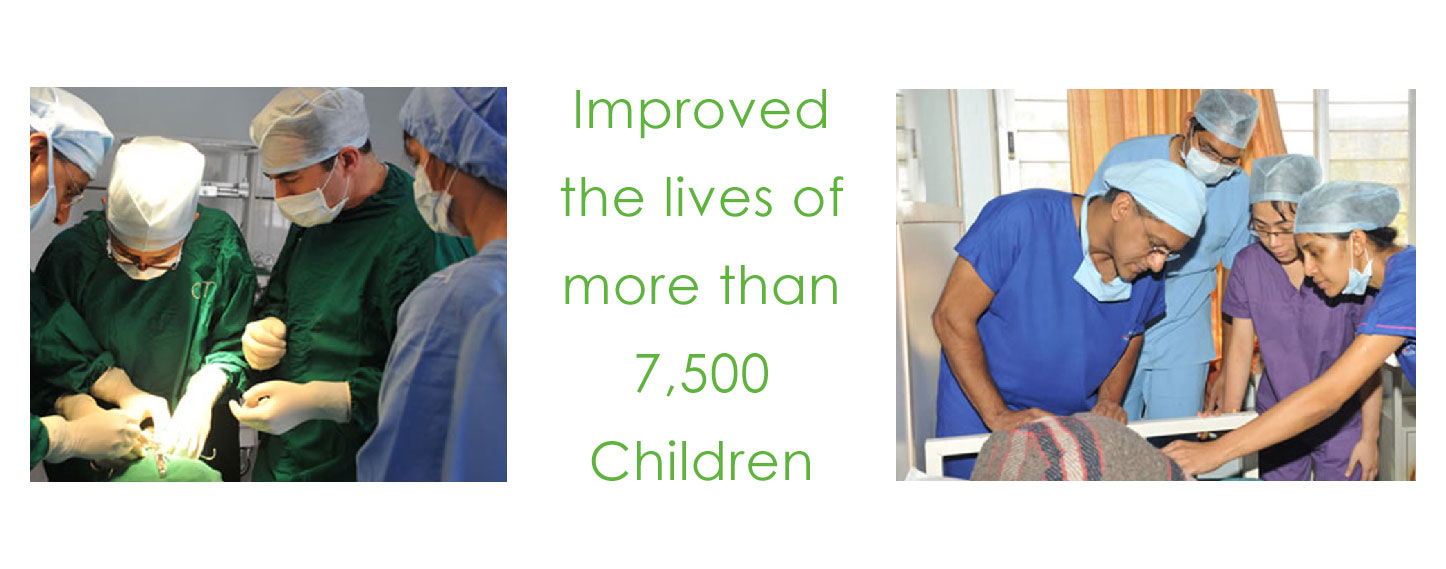
The absence of awareness among the public and health professionals. Besides, the cost itself: these surgeries are expensive and resourceconsuming. Even a free surgery funded by INGA Health Foundation
can cost up to Rs. 2.5 Lakhs on ano-profit, no-loss basis. The other challenge is the absence of trained surgeons and dedicated centres. Besides, the process of surgery iscomplicated; the space across
which one needs to work surgeriesis small in babies. To address these challenges, INGA Health Foundationinitiated a craniofacial surgerytraining programme for more than 30doctors.

These facial deformities lead to social stigma, poor self-esteem, speech impediments and hearing defects, among others. The more complicated craniofacial anomalies
might also compress the brain leading to lower IQ and under-par scholastic performance. They can also lead to the compression of theeyeball leading to partial or complete
blindness. In some conditions notonly is the external ear missing, butthe entire hearing system may becompromised leading to partial orcomplete deafness.

Enhancing awareness is number one. However, being in good health, and avoiding drugs and medication, during the first eight weeks of
pregnancy, and avoiding exposure to radiation can help reduce the chance of such deformities. Consanguineous marriages also increase the risk of
a malformed baby. INGA Health Foundation has tied up with rural work groups like Asha to enhance awereness on this subject.